SELF-DRIVING RADIOTHERAPY
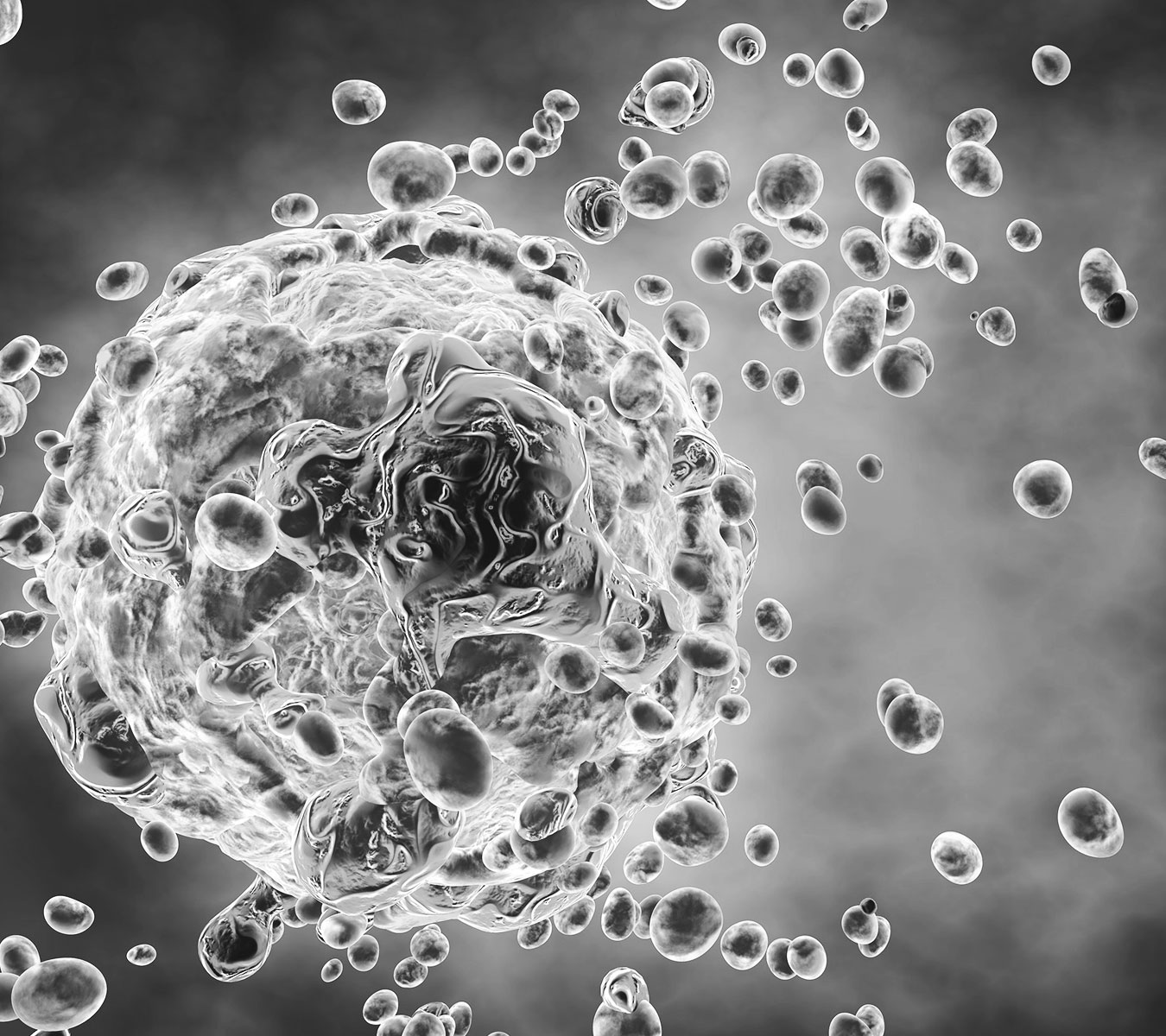
Cancer is talking.
We’re listening.
When radiopharmaceuticals are introduced into the body, cancer cells absorb them and create a biological beacon, which our machine uses to manage motion and treat solid tumors of any stage disease.
Learn About Emissions